The recent decision by the U.S. federal government to move cannabis from Schedule I to Schedule III under the Controlled Substances Act1 marks a significant inflection point for clinicians, researchers, and health systems. For decades, cannabis has been classified alongside dangerous and addictive substances. Schedule III status—shared by drugs with accepted medical uses and moderate to low potential for physical dependence—opens the door for further research and clinical use.
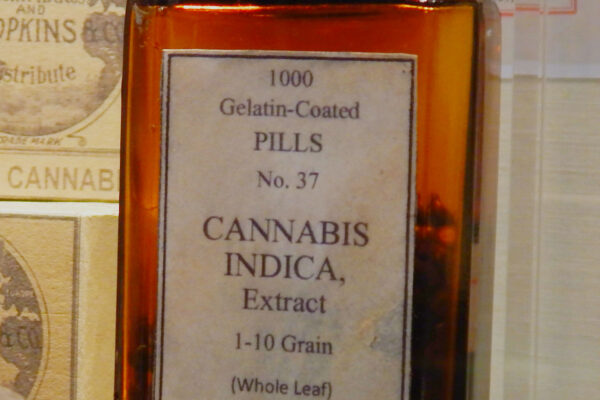
In the 19th and early 20th centuries, cannabis was listed in the United States Pharmacopeia and prescribed for conditions including pain, insomnia, and gastrointestinal disorders. Parke, Davis & Co. was a pioneering 19th-century pharmaceutical company that manufactured cannabis extracts (pictured here) for medicinal use, including products for migraines, neuralgia, and insomnia. More recently, cannabinoid-based pharmaceuticals2 3 have demonstrated efficacy in chemotherapy-induced nausea and vomiting, appetite stimulation in HIV/AIDS, and certain refractory epilepsies.
The reclassification to Schedule III has substantial implications for clinical research. Schedule I status imposed stringent registration requirements, limited manufacturing quotas, and complex approval pathways that disincentivized rigorous investigation. Under Schedule III, researchers may encounter fewer administrative barriers and greater willingness among academic medical centers to participate in trials. This shift should facilitate higher-quality randomized controlled trials examining pharmacokinetics, dosing strategies, safety profiles, and drug–drug interactions—areas that remain under-characterized in routine clinical practice.4
As stigma recedes and regulatory friction decreases, cannabis and cannabinoid-based therapies can be evaluated with the same methodological rigor applied to other Schedule III agents. The ultimate impact will depend on our collective ability to translate this regulatory change into clinical studies that identify the wide range of potential clinical uses and proper dosage. Rescheduling is not the finish line, but here at G3, we look forward to this new chapter in increasing understanding and access to a natural substance with significant potential clinical impact.
Resources
1. Controlled Substances Act, 21 U.S.C. § 801 et seq.
2. U.S. Food and Drug Administration. Prescribing information for dronabinol (Marinol, Syndros).
3. U.S. Food and Drug Administration. Prescribing information for Epidiolex.
4. National Academies of Sciences, Engineering, and Medicine. The Health Effects of Cannabis and Cannabinoids: The Current State of Evidence and Recommendations for Research. Washington, DC: National Academies Press; 2017.